Hi friends! It has come to my attention that people desire more information on both rosacea and perioral dermatitis. For that reason, I am going to do a little side-by-side comparison of these two common dermatologic skin disorders. If you believe you are struggling with either of these skin problems then you are not alone! As a dermatology physician assistant, I see and treat both conditions regularly in the clinic. In this article, I am going to discuss the appearance, common triggers of each, and most importantly how to treat them.
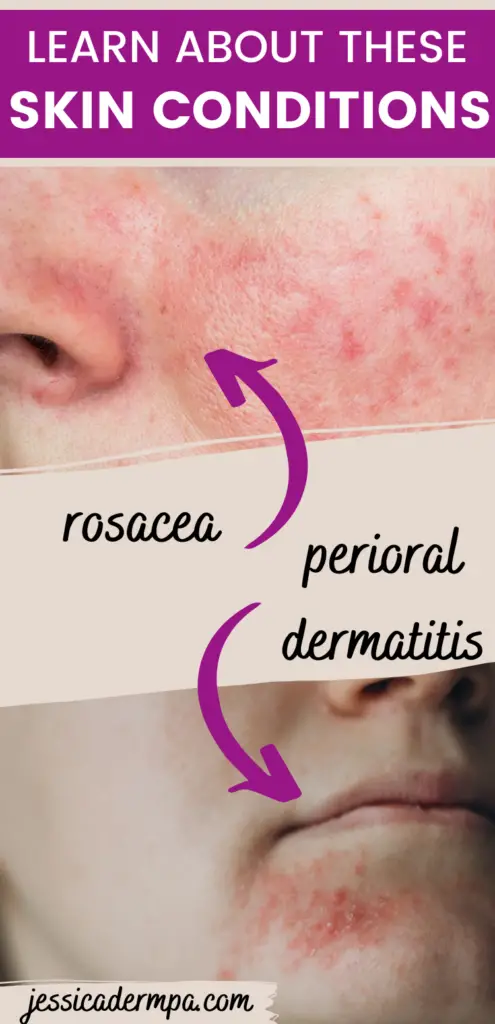
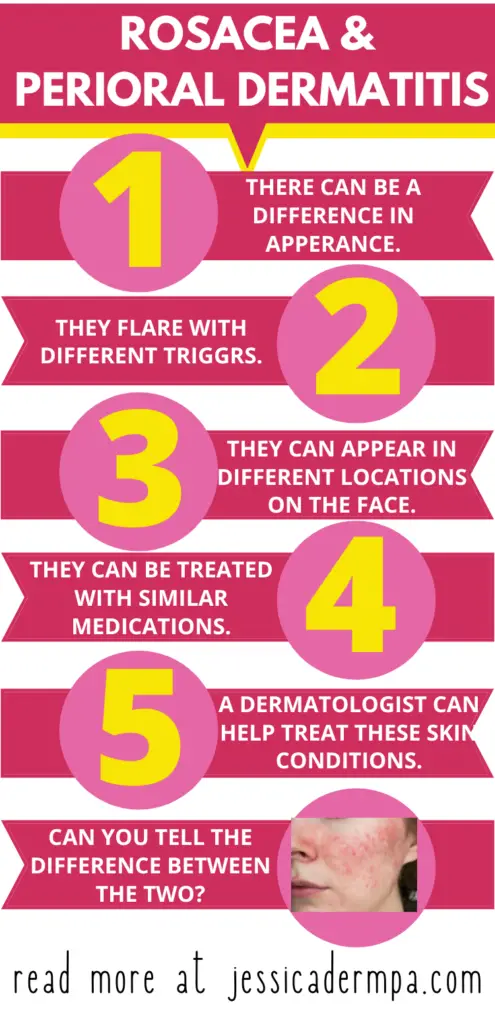
How to tell rosacea and perioral dermatitis apart
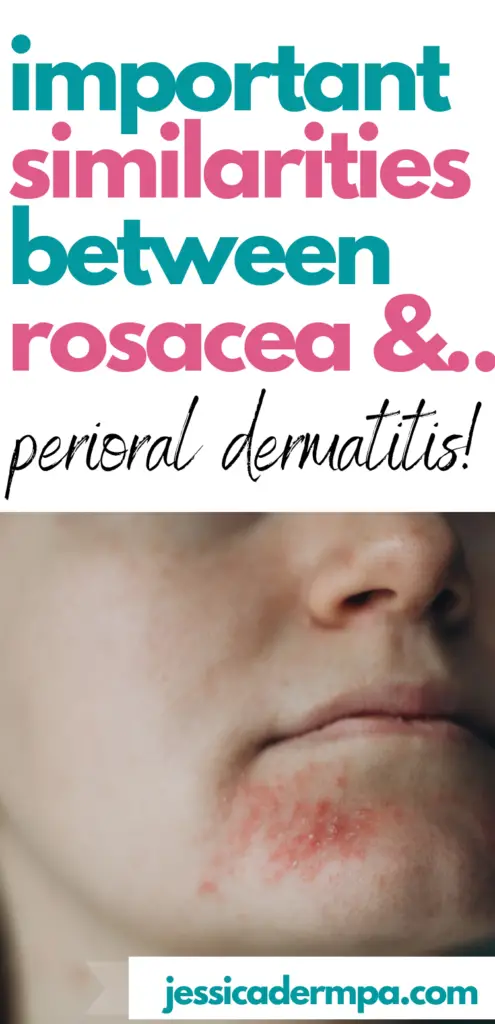
Rosacea and perioral dermatitis have two main components. They both cause rashes on the face. The rash can include dry flaking burning skin and acne-like bumps.
Rosacea
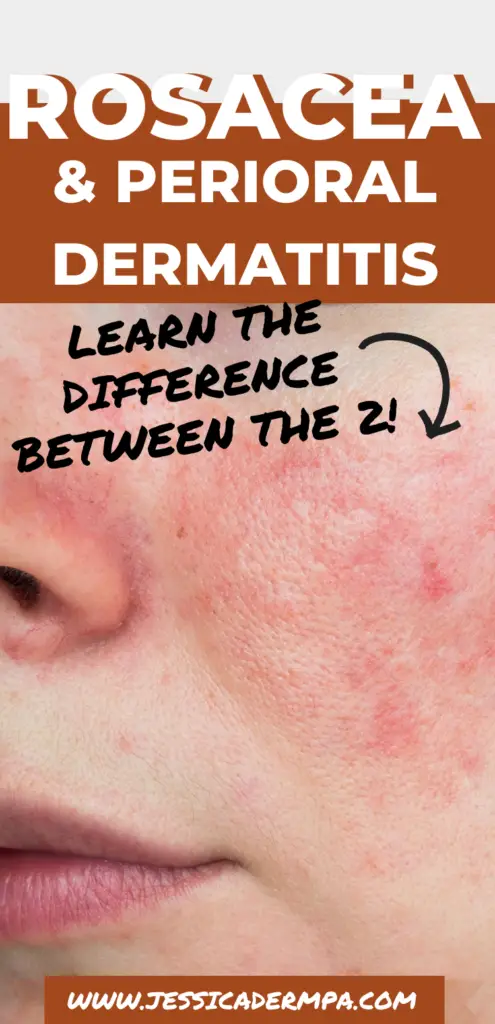
The main difference between the two is location on the face although this isn’t always 100% true in every individual. Most patients who come to me with rosacea experience it along their cheeks and nose. There’s typically an underlying pinkness to their face even when they’re not having a fare. You can also typically see telangiectasias along their cheeks, the medical word for superficial blood vessels.
It is important to note that rosacea can be more complex in severe cases, and different stages can look nothing like perioral dermatitis. For this article, we will be discussing the more common form of rosacea.
Perioral dermatitis
Perioral dermatitis is also sometimes known as periorificial dermatitis. Let’s discuss the difference. Perioral dermatitis typically implies a rash around the mouth. Perioralficial dermatitis can also imply a rash around the mouth but could also mean around the nose or eyes.
While the rashes can sometimes look similar, knowing where each skin disorder commonly appears on the face is beneficial for a clinical diagnosis.
The triggers of rosacea and perioral dermatitis
Rosacea
The first thing I counsel all my rosacea patients on is to avoid your triggers. Everyone with rosacea has different triggers that cause their skin to flare. Some of the more common ones are sun, stress, alcohol, spicy foods, and high intakes of caffeine or sugar.
If you don’t know what your trigger is then I recommend starting a journal. When your face flares write down everything you consumed in the past 24-48 hours including beverages. Also, what were you doing leading up to the flare? Were you outside for an extended period or maybe you were on a boat under shade but the wind was continuously whipping at your face?
After you have journaled for a few months take a look and see if you have any patterns. Avoiding triggers is sometimes difficult but other times it’s as simple as lowering your intake of a certain food or beverage.
Perioral dermatitis
Perioral dermatitis is typically due to a topical steroid (think hydrocortisone). For example, someone may have been prescribed a topical steroid because they have eczema and used that medication for an itch on the face. They then could have developed a rash and continued to apply the hydrocortisone causing a cycle that is hard to stop.
If someone has been using a topical steroid on their face for a while, when they stop it the rash almost always gets worse. This is known as a steroid withdrawal effect and there are non-steroidal medications that help if that is something you may be experiencing.
Other times perioral dermatitis could be due to a certain makeup product or too thick of an occlusive moisturizer. If you think this may be you then make sure you stop the product and then in the future ensure all of your makeup says non-comedogenic (safe for acne-prone skin).
I have also seen toothpaste especially very minty toothpaste or a recent fluoride treatment cause this type of rash. The good news is once you stop the offending agent and are started on the correct treatment, it should improve if not completely go away within a few weeks.
How to treat rosacea and perioral dermatitis
Rosacea
If you have rosacea then you have sensitive skin. The first thing is to use a gentle cleanser and moisturizer with SPF. I like Sulfalo soap which is a sulfur-based soap and gentle on the skin. For moisturizers with sunscreen try Elta MD Clear. They have a tinted or a non-tinted version.
Next, if you don’t have the pimples associated with rosacea and only the redness then you can either use a green-tinted makeup to cover it up, use a topical such as brimonidine (Mirvaso) or oxymetazoline (Rhofade), or invest in laser to target the blood vessels under the skin.
Be careful if your provider ever prescribes Mirvaso or Rhofade, they can be extremely helpful for some but they can, at times worsen rosacea or cause something called rebound redness, which is when you stop and the redness worsens.
Laser treatment is the only definitive treatment for the redness component of rosacea. It can be pricey and time-consuming but worth it for many.
What about the pimples? I’m glad you asked. The acne component of rosacea is in my opinion slightly easier to treat. There are many great topicals out there that can help. Keep in mind, that most of these are prescription-strength and will require an appointment with a medical provider.
Prescription-strength medications commonly used for treating rosacea are oral and topical antibiotics. Doxycycline is an oral antibiotic and can reduce the inflammatory component of rosacea. Add on a topical such as metronidazole or azelaic acid and you are in business. Occasionally a few different topical and oral combinations need to be tried before you find the one that works best for you. This is called the art of medicine!
Perioral dermatitis
A topical and or oral antibiotic is likely necessary to treat the perioral dermatitis. This is dependent on the severity of the condition as well as other factors including the age of the patient, allergies, and medical background.
First things first though. You have to stop whichever product is causing the rash in the first place. Once again, if you are using a topical steroid you should expect the rash to worsen before it improves. Nonsteroidal anti-inflammatories like tacrolimus and pimecrolimus can be helpful in the case of a steroid withdrawal flare. Just be warned, a lot of patients experience a burning sensation when they apply these medications.
Topical antibiotics that are normally used for the treatment of perioral dermatitis include metronidazole, erythromycin, and clindamycin. They are normally applied a few times a day to clean skin.
Sometimes oral medications are necessary to calm down more inflamed cases of perioral dermatitis or cases that are unresponsive to topicals. The oral antibiotics most commonly used are tetracyclines which include doxycycline and minocycline. These medications can have potential side effects like stomach upset, photosensitivity, esophageal irritation, and discoloration of the skin.
Treatment may take only a few weeks but other times it can take 2-3 months before someone reaches complete clearance of their rash. I usually recommend my patients against using any other products while trying to treat their perioral dermatitis besides whichever medication I prescribe. This is because another offending agent could increase the length of the necessary treatment to reach full clearance. Gentle cleansers for sensitive skin are typically fine to continue using. If you develop perioral dermatitis once you may be prone to recurrence at some point.
Final thoughts on rosacea and perioral dermatitis
There you have it, did you spot the similarities between these two skin conditions? If not I will break it down for you. Both rosacea and perioral dermatitis can look similar although location on the face can be a key distinguishing factor. While they can have different triggers, they are both inflammatory conditions that when avoiding the agent causing the trigger can help prevent further flares. Lastly, they can be treated similarly with topical and/or oral antibiotics.
Are you someone suffering from one or both of these skin conditions? Have you ever considered how they are somewhat related? Let us know your skincare routine in the comments below!
Related posts:
5 Common Skin Conditions Affected By Your Diet
The 10 Most Common Skin Disorders That Dermatology PAs Treat
*Disclaimer: Opinions expressed are solely my own and do not express the views or opinions of my employer. Information on this website is for education and entertainment purposes only. Content is my opinion. It is not substituted for your own doctor’s medical care or advice. One should not make any health or medical-related decisions based in whole or in part on any content on this site. Content is not intended to replace the services of a licensed, trained health professional. Content may not apply to you as an individual. Although I will update my website with current information, this website is not a definitive guide to dermatology.
View comments
+ Leave a comment