My second favorite season of the year is summer. Can you guess my favorite? I look forward to summer every year because it typically involves a week-long vacation. This summer, I went with my mom to London for a week! What I don’t look forward to in the summertime is the excessive heat we seem to be getting more and more frequently.
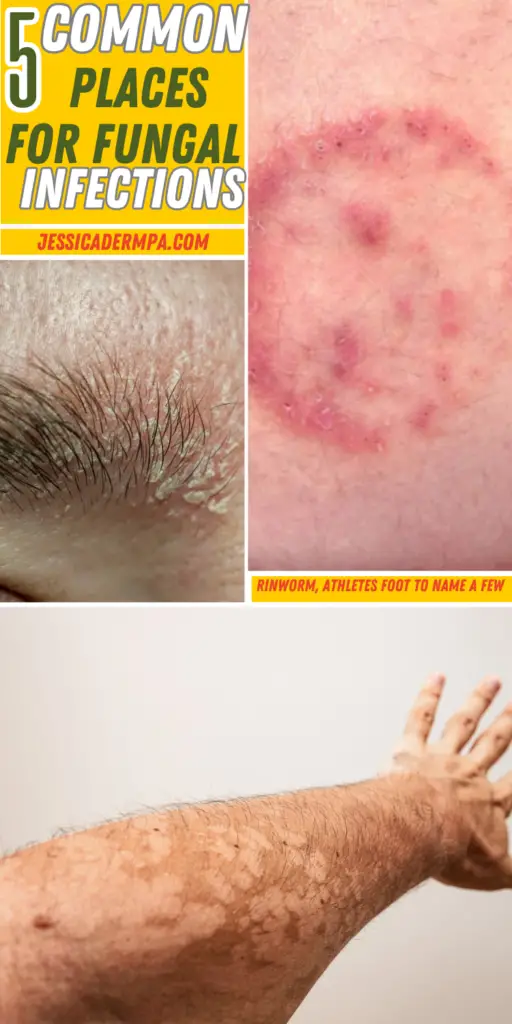
This summer has been especially bad in Memphis, TN, where I am located. The humidity is high, and with that comes patients complaining of a new rash. I would say roughly 1 out of 3 times the new rash that has popped up with all the extra sweat and sun is, in fact, a fungal infection. I am going to break down the 5 most common areas to get fungal infections in the summertime, and what can be used over-the-counter to help treat and prevent these annoying rashes.
1. Feet (Athlete’s Foot)
Overview: Athlete’s foot, or tinea pedis, is one of the most common fungal infections. It typically affects the skin between the toes but can also spread to the soles and sides of the feet. This infection is caused by dermatophytes, a type of fungus that thrives in warm, moist environments, such as sweaty socks and shoes, locker rooms, and public swimming pools.
Symptoms:
- Itching, stinging, or burning sensation between the toes or on the soles
- Red, scaly, and cracked skin
- Blisters or ulcers in severe cases
Prevention:
- Keep feet clean and dry, especially between the toes.
- Wear breathable shoes and moisture-wicking socks.
- Use antifungal powder or spray in shoes and on feet.
- Avoid walking barefoot in public areas like locker rooms and swimming pools.
Treatment:
- Over-the-counter antifungal creams or sprays (e.g., clotrimazole, miconazole).
- Prescription-strength antifungal medications for severe or persistent cases.
- Keeping feet dry and changing socks regularly.
2. Groin Area (Jock Itch)
Overview: Jock itch, or tinea cruris, is a fungal infection that affects the groin area, including the inner thighs and buttocks. It is more common in males but can also affect females. This infection is also caused by dermatophytes and is often exacerbated by sweating and friction from tight clothing.
Symptoms:
- Red, itchy rash in the groin area
- Circular, scaly patches with raised edges
- Skin peeling or cracking
Prevention:
- Maintain good hygiene by washing the groin area daily and after sweating.
- Keep the area dry and wear loose-fitting, breathable underwear.
- Avoid sharing towels, clothing, or athletic gear.
- Use antifungal powders to reduce moisture.
Treatment:
- Over-the-counter antifungal creams or powders (e.g., terbinafine, butenafine).
- Prescription-strength antifungal creams for more severe cases.
- Keeping the area clean and dry.
3. Scalp (Seborrheic Dermatitis)
Overview: Seborrheic dermatitis is a common condition that affects the scalp, causing red, scaly, and itchy patches. It is often associated with an overgrowth of Malassezia yeast, which thrives in oily areas of the skin. Although not purely a fungal infection, it is often treated with antifungal medications due to the involvement of yeast.
Symptoms:
- Red, flaky, and itchy patches on the scalp
- Dandruff (white or yellowish flakes)
- Greasy scales on the scalp
- Inflammation and irritation
Prevention:
- Wash hair regularly with a gentle shampoo to reduce oil buildup.
- Avoid using harsh hair products that can irritate the scalp.
- Manage stress, as it can exacerbate symptoms.
- Maintain a balanced diet to support overall skin health.
Treatment:
- Over-the-counter medicated shampoos containing ketoconazole, selenium sulfide, or zinc pyrithione.
- Prescription antifungal shampoos or creams for more severe cases.
- Topical corticosteroids to reduce inflammation and itching.
4. Body (Ringworm)
Overview: Ringworm, or tinea corporis, is a fungal infection that can affect any part of the body. Despite its name, ringworm is not caused by a worm but by dermatophytes. The infection is characterized by ring-shaped, red, and scaly patches that can appear on the trunk, arms, legs, or face.
Symptoms:
- Red, circular, and scaly patches with raised edges
- Itchy, inflamed skin
- Patches that grow and spread over time
Prevention:
- Maintain good personal hygiene by showering regularly and keeping skin clean and dry.
- Avoid sharing personal items such as towels, clothing, and sports equipment.
- Wear loose-fitting, breathable clothing to reduce sweating.
- Be cautious when handling pets, as they can carry the fungus.
Treatment:
- Over-the-counter antifungal creams or lotions (e.g., clotrimazole, terbinafine).
- Prescription-strength antifungal creams for more extensive infections.
- Keeping affected areas clean and dry.
5. Skin (Tinea Versicolor)
Overview: Tinea versicolor, also known as pityriasis versicolor, is a fungal infection caused by the Malassezia yeast, which naturally lives on the skin. This infection disrupts the normal pigmentation of the skin, resulting in small, discolored patches. It is more noticeable in the summer when affected areas do not tan evenly with the surrounding skin.
Symptoms:
- Small, discolored patches of skin, often lighter or darker than the surrounding skin
- Patches may appear white, pink, red, or brown
- Mild itching or scaling
Prevention:
- Keep the skin clean and dry, especially in humid conditions.
- Use antifungal shampoos as a body wash if prone to recurrent infections.
- Avoid excessive sun exposure, which can make the condition more noticeable.
- Wear loose-fitting, breathable clothing.
Treatment:
- Over-the-counter antifungal creams, lotions, or shampoos (e.g., selenium sulfide, ketoconazole).
- Prescription-strength topical or oral antifungal medications for more severe cases.
- Regular use of antifungal products to prevent recurrence.
Related post: 5 Rashes That Flare With Summer Sun, Heat, and Sweat
Conclusion
Fungal infections are a common summertime nuisance that can affect various parts of the body. Understanding the causes, symptoms, prevention, and treatment of these infections can help you stay healthy and enjoy the warmer months without discomfort. As a dermatology physician assistant, I recommend maintaining good hygiene, keeping skin dry, and using appropriate antifungal treatments to manage and prevent fungal infections. If you suspect a fungal infection, seek medical advice promptly to ensure effective treatment and prevent complications.
By following these guidelines, you can reduce your risk of fungal infections and enjoy a healthier, more comfortable summer.
*Disclaimer: Opinions expressed are solely my own and do not express the views or opinions of my employer. Information on this website is for education and entertainment purposes only. Content is my opinion. It is not substituted for your own doctor’s medical care or advice. One should not make any health or medical-related decisions based in whole or in part on any content on this site. Content is not intended to replace the services of a licensed, trained health professional. Content may not apply to you as an individual. Although I will update my website with current information, this website is not a definitive guide to dermatology.



View comments
+ Leave a comment